Abstract
Introduction: Diffuse large B-cell lymphoma (DLBCL) is one of the most prevalent Non-Hodgkin's Lymphoma (NHL) subtypes in the United States (US), with an estimated incidence of 5.6 cases per 100,000. DLBCL accounts for 30% of lymphomas in the US. Although it is an aggressive type of lymphoma, this is a highly curable disease with modern chemoimmunotherapy, with ~75% of patients achieving complete remission. Few studies have focused on age, race, ethnicity, health insurance, and performance status affecting survival rates. This study aims to evaluate the socioeconomic and sociodemographic disparities (age, race, ethnicity, median household income, geographic location, marital status) effecting mortality in adult patient population with DLBCL.
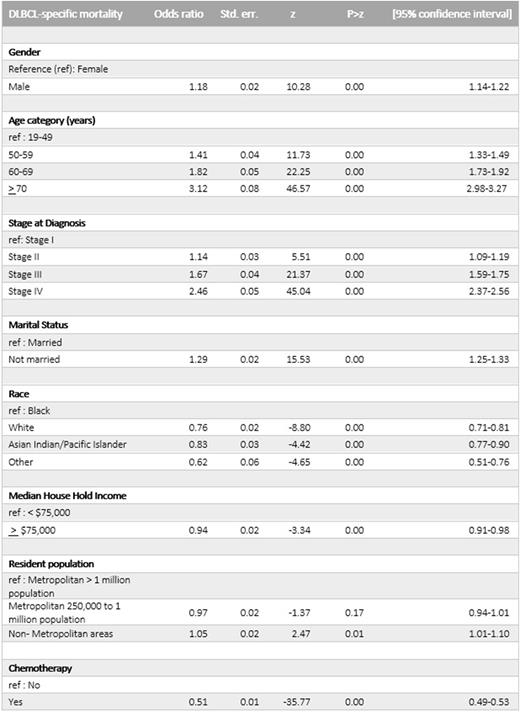
Methods: This is a retrospective cohort analysis of patients (>18 years) diagnosed with DLBCL, using data from the Surveillance, Epidemiology and End Results Plus (SEER plus) from 17 registries in the US spanning 20 years from 2000-2019. The SEER program collects data on cancer incidence and survival as population- based cancer registries across 22 U.S. diverse geographic regions. The primary outcome measure was cancer-specific mortality. Multivariable logistic regression was used to analyze clinical, demographic and socio-economic predictors of mortality. Factors significant on univariate analysis were included in the multivariable model. P< 0.01 was used as the threshold for significance due to large sample and multiple comparisons. Data analysis was conducted using Stata/BE version (Statacorp LLC, College Station, TX).
Results: Between 2000 -2019, there were a total of 113,173 patients (n=51,101(45.2%) females) diagnosed with DLBCL. Of these, 80,674 patients had documented Ann Arbor Staging (33.9% Stage IV, 16.8% Stage III, 20.4% Stage II, and 28.8% stage I), at the time of diagnosis. Of the final analyzed sample, 46.5% patients were ≥70yrs, 22.6% 60-69yrs, 15.6% 50-59yrs, and 15.3% ages 19-49yrs at the time of diagnosis. Whites (W) constituted 83.5%, Blacks 6.8%, and Asian Indian/Asian Pacific Islander (AI/API) 8.3%. B-symptoms were documented in the SEER plus database only from 2010 onwards (32.0% patients had ≥1 B-symptoms documented). 59.9% patients were from metropolitan areas with population size more than 1 million and 20.62% patients living in metropolitan areas with population size between 250,000 to 1 million, 19.51% includes patients living in Non-metropolitan areas. Median Household income inflation was adjusted to 2019; 66.6% had a median household income < $75,000, and 33.37% had a median household income ≥$75,000.
Of 113,173 patients, cancer-specific mortality was observed in 42,084 (37.5%) patients. On multivariable analysis, Male patients had higher mortality (Adjusted odds ratio (aOR),1.18; 95% CI, 1.14 -1.22) compared to females. Patients age ≥70 at the time of diagnosis, were associated with higher mortality (aOR,3.12; 95% CI 2.98-3.27) compared to the younger age group (19-49). Whites (W) (aOR,0.76; 95% CI 0.71-0.81) and Asian Indian/Pacific Islander patients (AI/PI) (aOR,0.83; 95% CI 0.77-0.90) had better overall survival compared to blacks. Patients diagnosed with Stage IV disease at the time of diagnosis had higher mortality (aOR,2.46; 95% CI 2.37-2.56) compared to Stage I patients. The unmarried patient population had lower survival (aOR,1.29; 95% CI 1.25-1.33). Income group ≥ $75,000 had lower mortality compared to lower income group (< $75,000) (aOR,0.94; 95% CI 0.91-0.98). Compared with patients living in Metropolitan areas with a population size > 1 million, Non-metropolitan areas had higher mortality (aOR,1.05; 95% CI 1.01-1.10). Patients who received chemotherapy had lower odds of death (aOR,0.51; 95% CI 0.49-0.53). In subgroup analyses, the association between sociodemographic factors and DLBCL specific mortality remained statistically significant across all groups analyzed.
Conclusions : Our study highlights the significant impact of various socioeconomic and sociodemographic disparities affecting the overall survival in DLBCL patients. Despite DLBCL-specific mortality having significantly decreased over the years, black patients, patients with lower household Income, living in non-metropolitan areas and smaller counties with limited access to health care, have considerably higher mortality risk in DLBCL after adjusting for various clinical predictors.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.